Definition
 |
| Ascites with umbilical hernia. |
Ascites is the accumulation of excess fluid in the peritoneal cavity, most commonly caused by liver cirrhosis.
Physical finding and Clinical presentation
- Important information to elicit within history
- Viral hepatitis
- Alcoholism
- Increasing abdominal girth, umbilical hernia
- Increasing lower extremity edema
- Intravenous drug use
- Sexual history (i.e., men who have sex with men)
- History of transfusions
- Important physical examination findings
- Bulging flanks
- Flank dullness to percussion
- Fluid wave on abdominal examination
- Lower extremity edema
- Shifting dullness “succusion splash” on abdominal examination
- Physical signs associated with liver cirrhosis: spider angiomas, jaundice, loss ofbody hair, Dupuytren’s contracture, muscle wasting, bruising, palmar erythema, gynecomastia, testicular atrophy, hemorrhoids, caput meduse
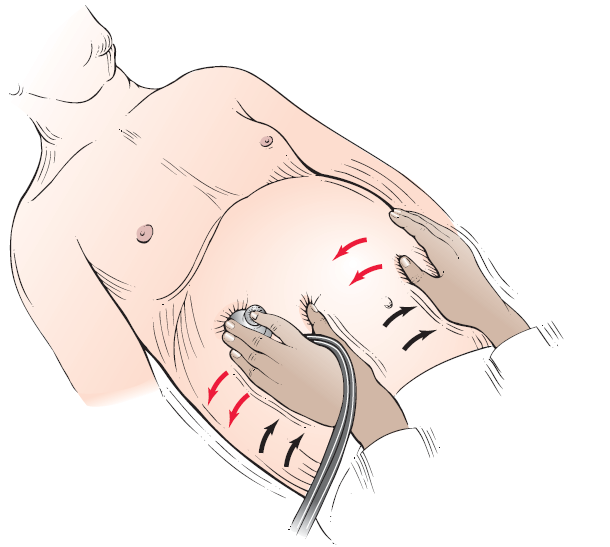 |
| "Succusion splash” technique for assessing distention of abdominal viscera. |
Cause
Pathophysiology of ascites: increased hepatic resistance to portal flow leads to portal hypertension. The splanchnic vessels respond by increased secretion of nitric oxide causing splanchnic artery vasodilation. Early in the disease increased plasma volume and increased cardiac output compensate for this vasodilation. However, as disease progresses the effective arterial blood volume decreases causing sodium and fl uid retention through activation of the renin-angiotensin system. The change in capillary pressure causes increased permeability and retention of fluid in the abdomen.
Differential Diagnosis
- Chronic parenchymal liver disease, leading to portal hypertension
- Peritoneal carcinomatosis
- Congestive heart failure
- Peritoneal tuberculosis
- Nephrotic syndrome
- Pancreatitis
Laboratory Tests
- Initial evaluation should always include:
- Diagnostic paracentesis. Laboratory tests on this fluid should include a CBC with differential, albumin, total protein, culture and a Gram stain. Optional tests on paracentesis fluid (depending on patient’s history) include amylase, LDH, acid-fast bacilli and glucose levels
- AST, ALT, total and direct bilirubin, albumin, alkaline phosphatase, GGTP
- CBC, coagulation studies
- Electrolytes, BUN, creatinine
- A serum to ascites albumin gradient (SAAG) should be calculated in all patients. If the SAAG is greater than 1.1, the cause of ascites can be attributed to portal hypertension. If SAAG is less than 1.1, a nonportal hypertension etiology of ascites must be sought.
Imaging studies
- Endoscopy of the upper GI tract to evaluate for esophageal varices if ascites is secondary to portal hypertension.
- Abdominal ultrasound is the most sensitive measure for detecting ascitic fl uid; a CT scan is a viable alternative.
- Liver biopsy in select patients (i.e., those with portal hypertension of uncertain etiology).
Treatment
- Sodium-restricted diet (maximum 60-90 milliequivalents per day).
- Fluid restriction to 1 liter per day in patients with hyponatremia.
- Patients with moderate-volume ascites causing only moderate discomfort may be treated on an outpatient basis with the following diuretic regimen: spironolactone 50-200 mg daily or amiloride 5-10 mg daily. Add furosemide 20-40 mg per day in the fi rst several days of treatment, monitoring renal functions carefully for signs of prerenal azotemia (in patients without edema goal weight loss is 300-500 grams/ day, in patients with edema 800-1000 grams/day).
- Patients with large-volume ascites causing marked discomfort or decrease in activities of daily living may also be treated as outpatients if there are no complications. There are two options for treatment in these patients: (1) largevolume paracentesis or (2) diuretic therapy until loss of fluid is noted (maximum spironolactone 400 mg daily and Lasix 160 mg daily). There is generally no difference in longterm mortality; however paracentesis is faster, more effective,and associated with fewer adverse effects.
- Five percent to 10% of patients with large-volume ascites will be refractory to high-dose diuretic treatment. Treatment strategies include repeated large-volume paracentesis with infusion of albumin every 2-4 weeks or placement of a transjugular intrahepatic portosystemic shunt (TIPS).













